Data Visualization Masters Thesis
The written content, research, data analysis, user experience research, and designs below were all produced for my thesis.
Position: MPS Candidate, Maryland Institute College of Art, Dec. 2018
Role: Data Analyst, Writer, Designer
There's Something About Mary

Celebrating Mary’s 28th birthday in 2016 (Left: Me, Right: Mary)
This is a story about data. It’s about cancer and science and the power of populations in research. It is also the story of the life and death of my best friend Mary Billington. After her death from cancer and still full of our many years together, I needed to learn more about the various cancers she had, so with the full consent of her family I started researching her history. I learned that Mary’s life and death was an intertwining story of genetics and cancer; seemingly separate strands that, in retrospect, were actually not at all separate. These strands flow together to create a unique and unified story—that all starts with Mary.
THE FIRST STRAND: THE MISSING GENE
Mary was born without the RB1 gene. The RB1 gene, located in Chromosome 13, provides instructions for making a protein called pRB. This protein acts as a tumor suppressor, which means it regulates cell growth and keeps cells from dividing too fast or in an uncontrolled way. Without this gene, Mary’s body didn’t have the protein needed to suppress tumors. Retinoblastoma is one of the known health conditions resulting from a chromosomal change in chromosome 13.
What is retinoblastoma? Retinoblastoma is an ocular cancer that begins in the retina, the part of one’s eye that senses light and sends signals through the optic nerve to the brain, which then interprets them as images.
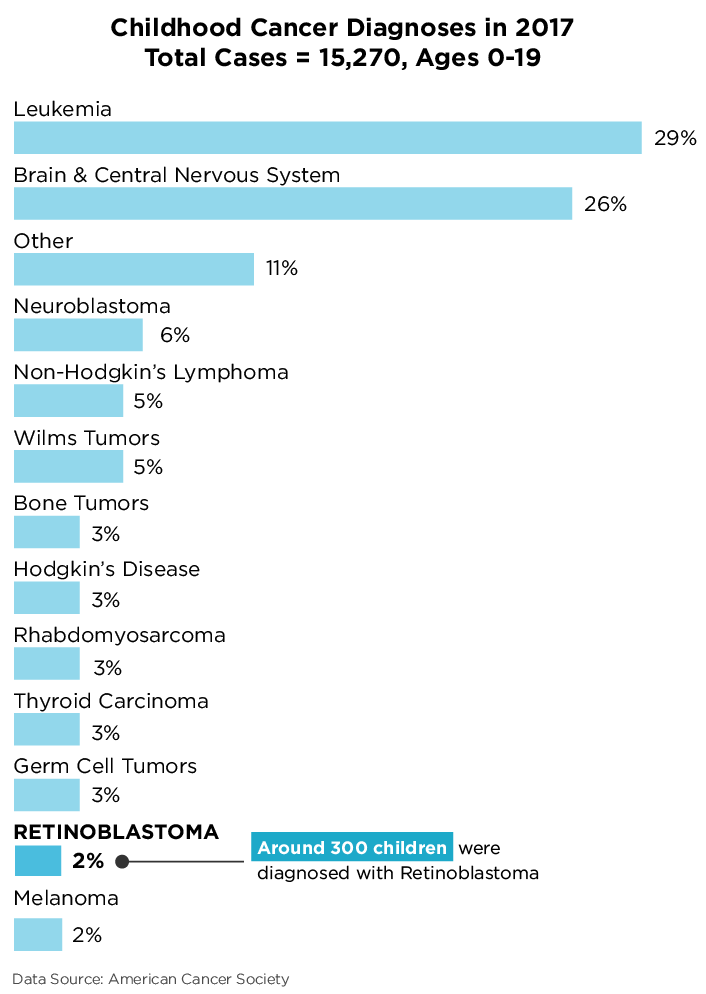
In 2017, there were 15,270 cases of pediatric cancer diagnosed in children ages 0-19. Of these, more than half were leukemias, brain cancers, and cancers of the central nervous system. Retinoblastoma accounted for 2 percent of the pediatric cancers — approximately 300 cases. While 2 percent doesn't seem like much, in the world of data, it’s not considered rare; 300 cases a year creates enough data for researchers to work with in statistically significant conditions.
Retinoblastoma provided the conceptual framework for how doctors and researchers started seriously exploring the links between heredity and the incidence of specific cancers. The first serious researcher of retinoblastoma, Dr. Alfred Knudson, used this cancer in young children as the model because it seemed to have incidence rates that were not complicated by the issues of older children and adults. Gene mutation or absence was determined to pass genetically and lead to retinoblastoma. It was then determined to lead to the annual increase in its incidence — 7 percent since the 1970s. So a missing gene was found to lead to a known cancer, which led to its recognition as a pediatric cancer and explained its origins.
Mary had been born with apparent good health, and prenatal genetics testing in the 1980s was limited to high-risk populations, particularly the chassidic Jewish communities from Eastern Europe who had settled in America after the Holocaust and whose close family marriages were found to have brought Tay-Sachs Disease and other genetic illnesses from very low incidence to statistically significant levels. But not, generally, others. Thus, Mary’s family didn’t know she born without the RB1 gene, and Mary was otherwise born healthy. From the vantage of statistical objectivity, not knowing any of her family’s genetic history, Mary stood no more than a 0.01 percent chance of being born with retinoblastoma; there are approximately 400 diagnoses per year in 4 million live births. Add to that, she had it in both eyes, which only occurs in 75 of the 400 diagnoses every year — or less than 1 in 5 of the 0.01 percent. But having been beaten by these odds, she was diagnosed and radiation was started at 5 months old.
In the 1980s, radiation was the only practiced option to cure retinoblastoma, although it was complicated and removed from standard practice much later when it was learned, in this and many other cancers, that the radiation caused its own cancers. This proved to be particularly true in patients who are missing the RB1 gene, however radiation was the only option available to save Mary’s vision and provide Mary with future decades.
THE SECOND STRAND: THE CONSEQUENCE OF TREATMENT
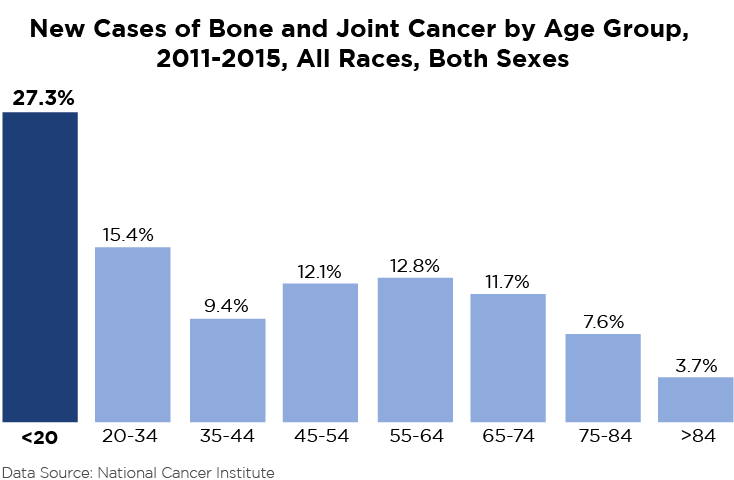
At age 12, Mary was diagnosed with Osteogenic Sarcoma (Osteosarcoma), the second strand of this story. Osteosarcoma is a cancer that starts in the bone and forms when a young person grows new bone tissue — in Mary’s case, her right sinus. Most osteosarcomas occur in children and young adults between 10 and 30 years old. During 2011-2015, the highest group of new cases of bone and joint cancers were under the age of 20. While the cause for osteosarcoma is unknown and represents less than 1 percent of all cancers diagnosed in the United States, it has been linked to patients who have a defective or missing tumor suppressor gene — in Mary’s case, RB1. People who have received radiation are also more likely to develop osteosarcoma, so while Mary’s additional diagnosis was a shock to her family, it wasn’t to her doctors - once the various incidence variables are compounded with her existing retinoblastoma and radiation history, not surprising.
During the spring of 2000, Mary underwent extensive surgery to remove the tumor in her right sinus, followed by a year of chemotherapy. Removing the tumor meant removing the bone structure that supported her eye, and her eye was removed at the same time, leading to the first appearance of the patch she wore for the rest of her life.
THE THIRD STRAND: THE LIKELY RECURRENCE
After the osteosarcoma and treatment, Mary was cancer-free for a few years. Halfway through her freshman year of high school, a routine chest scan found bone cancer in her heart. Apparently, and again in the face of low odds, a cancerous cell from the sinus tumor had survived, traveled through her bloodstream, and lodged in her heart.
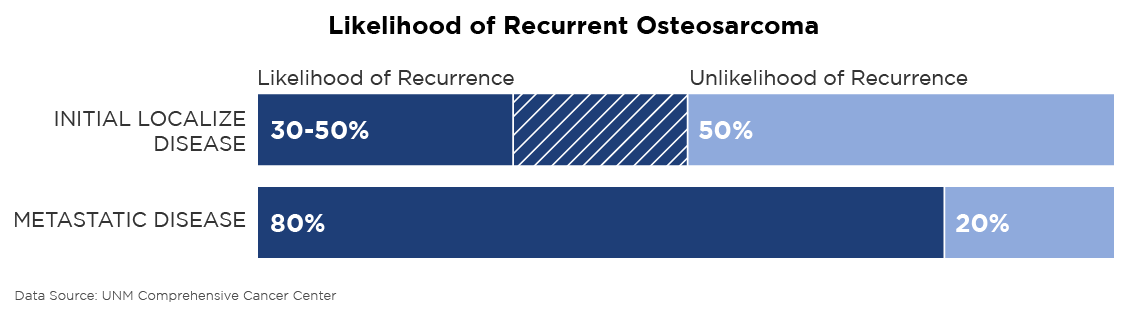
This time, unlike the retinoblastoma, she was now fighting tougher odds: recurrent osteosarcoma recurs in 30-50 percent of patients with initial localized disease like Mary’s (and in 80 percent of patients who already have metastatic disease, cancer spread throughout their bodies). Days after her 15th birthday, she underwent open heart surgery and another year of chemotherapy.
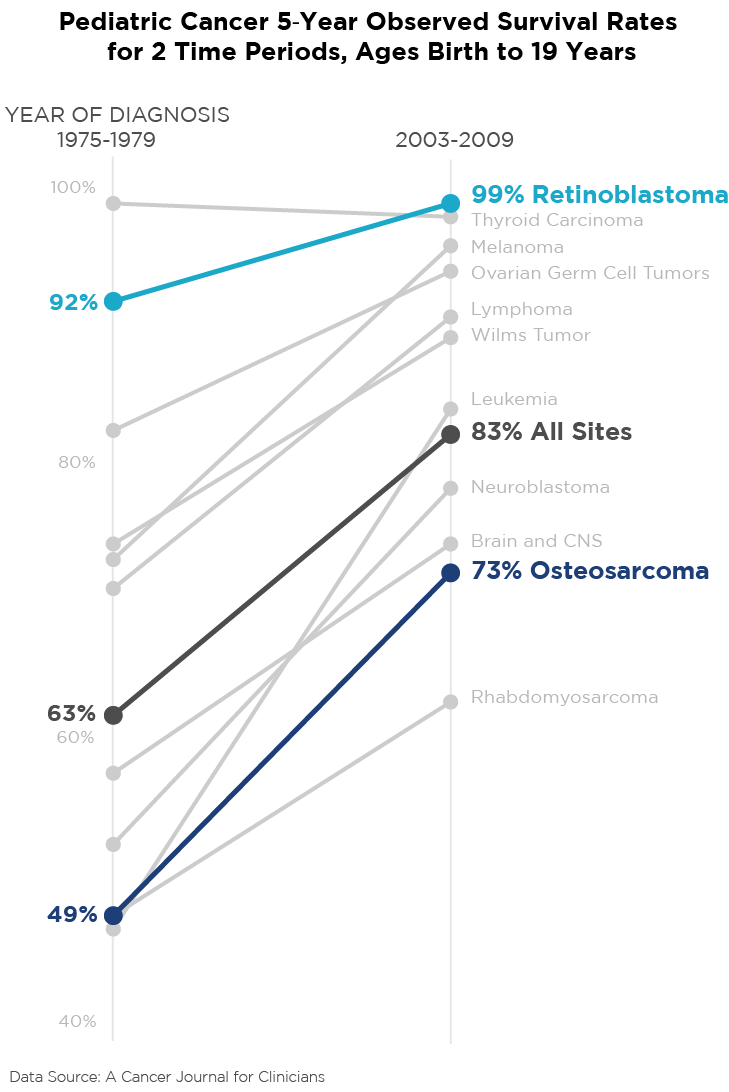
Retinoblastoma is essentially curable and has been for many years. Although the five-year survival rates of osteosarcoma were significantly improving from the mid 1970s to early 2000s, it could still be fatal in more than one quarter of the diagnoses. Mary had a 73 percent chance of surviving five years if osteosarcoma had remained her only problem. While many pediatric cancer patients benefited from 25 years of research, some still suffered. If Mary had been diagnosed in the late 1970s, she would have faced — at best — even odds of surviving five years. Twenty-five years later, her odds were 3-to-1 in her favor. The mean 5-year survival rate of all pediatric cancers went from 63 percent to 83 percent, showing the incredible advances in medical research, even though there are still thousands of dying children in that population mean. For the next 12 years, Mary was ahead of the survival rates for both retinoblastoma and osteosarcoma. She was cancer-free through college at Barnard College and graduate school at Harvard University, and her early working years, all the while living a life where she constantly strived for more, not just personally but professionally too - working politically on behalf of education policy and children with cancer, for the next twelve years. She knew the threat of a potentially shortened life would never go away, and demanded 150 percent from every day.
THE FOURTH STRAND: THE MYSTERIOUS DETECTION
In the fall of 2015, Mary found a lump in her breast and was diagnosed with Stage II breast cancer. As Mary herself stated, “that diagnosis was more of a mystery than the others. While unfortunate, the three previous times there was story arc there — they made a certain amount of sense, and the breast cancer really didn’t.“ As we know, approximately one in eight women will develop invasive breast cancer, the most common diagnosis of cancer for women. And her specific diagnosis was invasive ductal carcinoma (IDC), in which tumor growth occurs in a milk duct and invades the fatty tissue of the breast, the most common form of breast cancer.
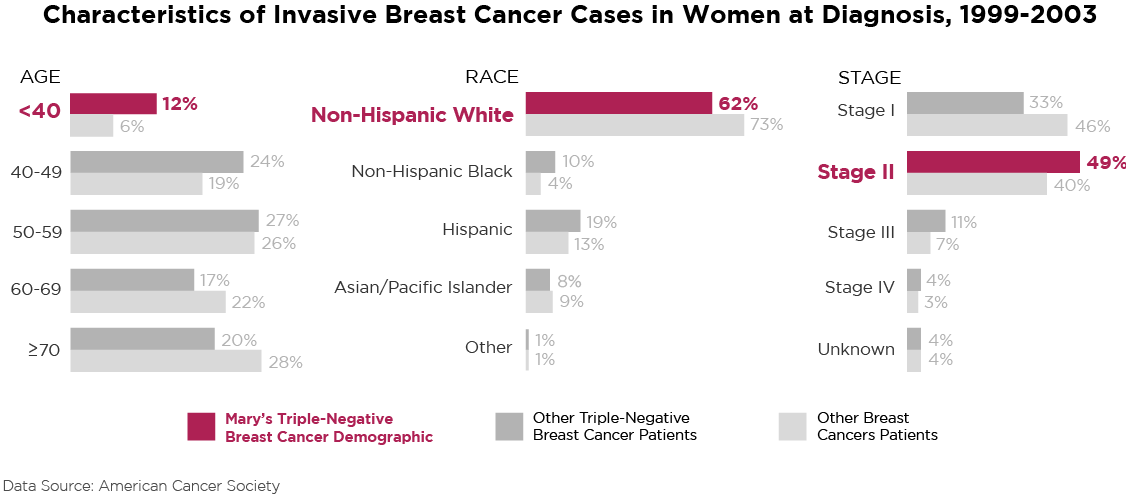
However, as with the first three strands of this story, Mary’s diagnostic situation did not fit the easily treatable norm. She was found to have triple-negative IDC. Breast cancer isn’t one disease — it’s a family of subtypes, and triple-negative breast cancer is a less common subtype. Approximately 10 to 20 percent of women who receive a breast cancer diagnosis test negative to the typical receptors, resulting in the triple-negative subtype.
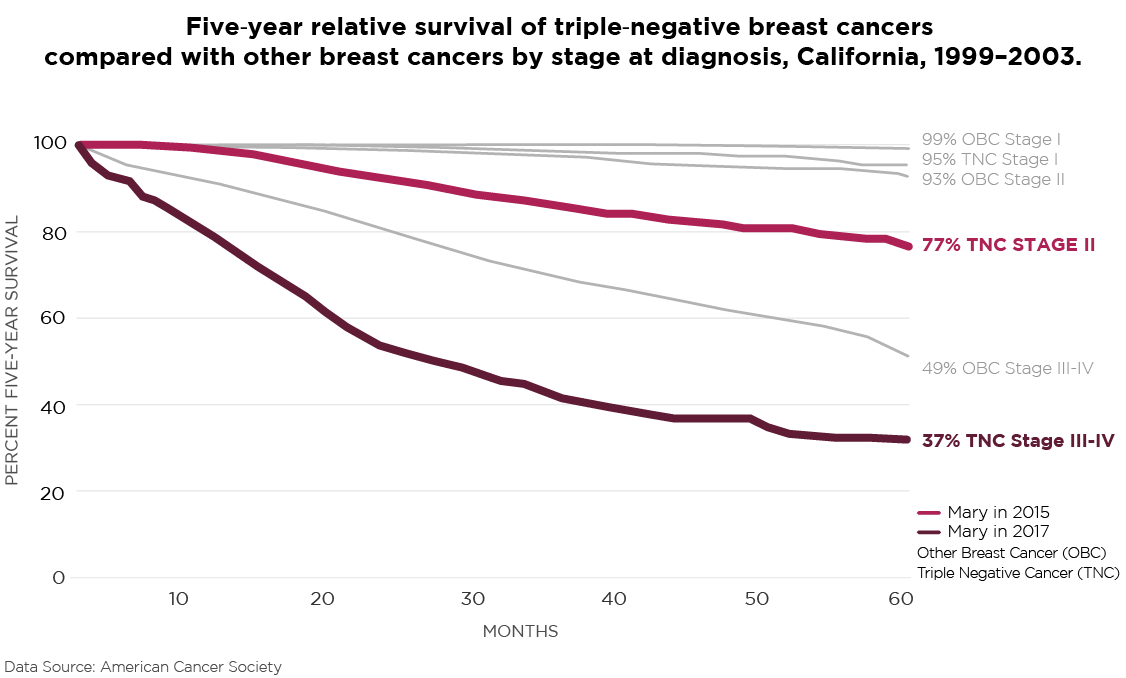
Being under 40 years of age is the least common age group within the characteristics of invasive breast cancer cases, and its standard treatment is mastectomy, even for younger women, because triple-negative breast cancer, an aggressive cancer with few treatment options, carries a high recurrence rate, particularly within the first three years. Thus, at 27, Mary had a double mastectomy and underwent yet another year of chemotherapy. With Mary’s particular way of having bad results follow every step, the recurrence probability was a scary thought for all of us.
THE FINAL STRAND: THE LAST RODEO
In November 2017, Mary’s breast cancer returned with a vengeance, spreading to her lymph nodes, liver, spine, and a few other spots throughout her body. She’d been dealing with back pain for about six weeks — back pain she learned was the result of tumors infiltrating and eventually collapsing a couple of vertebrae in her spine. A few weeks later, she was diagnosed with stage IV metastatic breast cancer.
As Mary stated in an email during that period, “the pathology of this tumor matches the pathology of the tumor that was removed during my breast cancer surgery last year. This means that one or more microscopic cancer cells were not successfully removed during surgery; they survived six months of chemotherapy; and have spent the past year or so growing and spreading throughout my body.” From this point until the end, Mary became a classic stage IV patient, dealing with each new and unfortunate step of the cancer taking over and destroying her body, leading to organ failure and, finally, her death in March 2018.
Mary’s unique story is one of cancer, science, and data. It started with her missing the RB1 gene at birth, which made her body less able to suppress tumors. The missing RB1 gene led to the retinoblastoma, whose treatment caused osteosarcoma. And then much later, with Mary still defenseless to tumors, breast cancer took hold. But Mary’s story is also about a fighter who refused to give up even though it turned out to be a battle she genetically couldn’t win.
POSTSCRIPT
There was something about my best friend Mary, she was the world’s best fighter. She was fond of saying that cancer taught her how to define her focus and her life’s goals. She was known for reciting the quote, “life is 10 percent what happens to you, and 90 percent your reaction to it.” While this story is about her less than ideal 10 percent, the impact she made on my life is the 90 percent of how she reacted to it. On August 12, 2017, she tweeted “‘Beating cancer’ doesn't have to be defined in medical terms. I often think, if I ever lose the desire to laugh, then cancer will have won.” She was making jokes up to her last day and that was her 90 percent defeating the 10 percent.
ENDNOTES
Bauer, K. R., Brown, M., Cress, R. D., Parise, C. A., & Caggiano, V. (2007). Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype. Cancer, 109(9), 1721-1728. doi:10.1002/cncr.22618
Bauer, K. R., Brown, M., Cress, R. D., Parise, C. A., & Caggiano, V. Cancer, 109(9), 1721-1728.
Cancer Facts & Figures 2018 (Rep.). (n.d.). Atlanta: American Cancer Society.
Chang, K. (2016, July 16). Dr. Alfred G. Knudson, the ‘Mendel of Cancer Genetics,’ Dies at 93. New York Times. Retrieved October 15, 2018, from https://www.nytimes.com/2016/07/15/science/dr-alfred-g-knudson-the-mendel-of-cancer-genetics-dies-at-93.html
Chromosome 13 - Genetics Home Reference - NIH. (n.d.). Retrieved from https://ghr.nlm.nih.gov/chromosome/13#conditions
Giacinti, C., & Giordano, A. (2006, August 28). RB and cell cycle progression. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16936740
Invasive Ductal Carcinoma: Diagnosis, Treatment, and More. (n.d.). Retrieved from https://www.breastcancer.org/symptoms/types/idc
Key Statistics for Osteosarcoma. (n.d.). Retrieved from https://www.cancer.org/cancer/osteosarcoma/about/key-statistics.html
Mirabello, L., Troisi, R. J., & Savage, S. A. (2009). Osteosarcoma incidence and survival rates from 1973 to 2004. Cancer, 115(7), 1531-1543. doi:10.1002/cncr.24121
Retinoblastoma. (n.d.). Retrieved from https://www.stjude.org/disease/retinoblastoma.html
Retinoblastoma. (2018, August 09). Retrieved from https://www.mayoclinic.org/diseasesConditions/retinoblastoma/symptoms-causes/syc-20351008
TripleNegativeBreastCancerOutlook: Survival Rates. (n.d.). Retrieved from https://www.healthline.com/health/triple-negative-breast-cancer-outlook-survival-rates-stage#definition
Ward, E., PhD, DeSantis, C., MPH, Robbins, A., MD PhD, Kohler, B., MPH, & Jemal, A., DVM PhD. (2014). Childhood and adolescent cancer statistics, 2014. A Cancer Journal for Clinicians, 79-82. doi:10.3322/caac.21219
Ward, E., PhD, DeSantis, C., MPH, Robbins, A., MD PhD, Kohler, B., MPH, & Jemal, A., DVM PhD. (2014). Childhood and adolescent cancer statistics, 2014. A Cancer Journal for Clinicians, 79-82. doi:10.3322/caac.21219